
Προοίμιο Ι – Η Σιωπή πριν από την Πτώση
Πριν από την πτώση υπήρχε σιωπή. Όχι κενό, όχι απουσία, όχι αμηχανία. Υπήρχε σιωπή γεμάτη, πυκνή, κατοικημένη. Σιωπή που δεν ζητούσε να μιλήσει, γιατί δεν της έλειπε τίποτε. Εκείνη η σιωπή δεν ήταν άγνοια· ήταν κοινωνία. Δεν ήταν αδυναμία λόγου· ήταν πληρότητα παρουσίας. Ζούσα μέσα της χωρίς να τη σκέφτομαι. Δεν υπήρχε «εγώ» για να την αναλύσει, ούτε «εσύ» για να την αμφισβητήσει. Υπήρχε μόνο το «μαζί», και αυτό αρκούσε.
Στη σιωπή εκείνη ο Θεός δεν ακουγόταν ως φωνή. Ήταν αναπνοή. Ήταν ρυθμός ζωής. Ήταν το φως που δεν τυφλώνει, γιατί δεν συγκρίνεται με το σκοτάδι. Ήταν το νόημα πριν τη λέξη. Και εγώ ήμουν μέσα σε αυτό, όχι ως παρατηρητής, αλλά ως μέτοχος. Δεν υπήρχε ανάγκη να καταλάβω, γιατί δεν υπήρχε απόσταση. Όλα ήταν παρόντα χωρίς να κατονομάζονται. Όλα ήταν δοσμένα χωρίς να διεκδικούνται.
Θυμάμαι αυτή τη σιωπή σαν μνήμη που δεν έζησα με το σώμα μου, αλλά με την ψυχή μου. Τη θυμάμαι γιατί την έχασα. Και μόνο ό,τι χάνεται αποκαλύπτει τι ήταν. Εκεί δεν υπήρχε φόβος, γιατί δεν υπήρχε μέλλον να απειλεί. Δεν υπήρχε ενοχή, γιατί δεν υπήρχε ρήξη. Δεν υπήρχε ερώτηση, γιατί δεν υπήρχε αμφιβολία. Η αλήθεια δεν χρειαζόταν υπεράσπιση· ανάσαινε.
Η σιωπή πριν από την πτώση δεν ήταν ουδέτερη. Ήταν ιερή. Όχι γιατί κάποιος την όρισε έτσι, αλλά γιατί ήταν χώρος Θεού. Και κάθε τι που είναι χώρος Θεού δεν χρειάζεται τελετουργία· είναι η ίδια η τελεία πράξη ζωής. Εκεί δεν υπήρχε λατρεία ως πράξη, γιατί όλη η ύπαρξη ήταν λατρεία. Ο άνθρωπος δεν στεκόταν απέναντι στον Θεό· στεκόταν εντός Του. Όχι ως ταύτιση, αλλά ως κοινωνία αγάπης.
Σε εκείνη τη σιωπή δεν υπήρχε ανάγκη επιλογής. Όχι γιατί έλειπε η ελευθερία, αλλά γιατί η ελευθερία δεν είχε ακόμα διασπαστεί σε δυνατότητες. Η ελευθερία ήταν σχέση, όχι απόφαση. Ήταν παραμονή, όχι ρίσκο. Και εγώ, ως άνθρωπος, ήμουν ολόκληρος χωρίς να το ξέρω. Δεν μετρούσα τον εαυτό μου. Δεν με χώριζα. Δεν οριζόμουν. Απλώς ήμουν.
Αυτή η σιωπή είναι το μέτρο της πτώσης. Όχι ο καρπός. Όχι η εντολή. Όχι η παράβαση. Το μέτρο είναι η απώλεια της σιωπής. Γιατί όταν χάνεται η σιωπή, γεννιέται ο θόρυβος του «εγώ». Και τότε αρχίζει η ανάγκη για λόγο, για εξήγηση, για δικαίωση. Τότε ανοίγει ο χώρος για άλλες φωνές. Και τότε, χωρίς να το καταλάβω, η σιωπή που ήταν Θεός, γίνεται κενό που ζητά να γεμίσει. Εκεί, ακριβώς εκεί, θα μιλήσει ο όφις.
Προοίμιο ΙΙ – Η Σιωπή πριν από την Πτώση
Η σιωπή πριν από την πτώση δεν έσπασε από κάποια κραυγή. Δεν ράγισε από κάποια σύγκρουση. Άρχισε να λεπταίνει ανεπαίσθητα, σαν ανάσα που χάνει το ρυθμό. Κανείς δεν φώναξε μέσα στην Εδέμ. Κανείς δεν ύψωσε φωνή. Η ρωγμή δεν μπήκε με θόρυβο· μπήκε με μετατόπιση. Και αυτή η μετατόπιση δεν φαινόταν απ’ έξω. Γινόταν εντός μου.
Δεν χάθηκε αμέσως η σιωπή. Αλλαξε ποιότητα. Από πλήρης έγινε εύθραυστη. Από κατοικημένη έγινε επιφυλακτική. Και εκεί, μέσα σε αυτή τη λεπτή αλλαγή, γεννήθηκε κάτι που δεν υπήρχε πριν: η ανάγκη να ακούσω αλλιώς. Όχι να ακούσω περισσότερο, αλλά να ακούσω κάτι επιπλέον. Όχι τον Θεό όπως Τον ζούσα, αλλά έναν λόγο που ερχόταν δίπλα Του. Όχι απέναντί Του ακόμη. Δίπλα Του.
Κατάλαβα αργότερα ότι η πτώση δεν άρχισε με ανυπακοή, αλλά με περιέργεια. Όχι παιδική, αλλά υπαρξιακή. Η περιέργεια αυτή δεν ρωτούσε «ποιος είναι ο Θεός», αλλά «τι άλλο υπάρχει πέρα από Αυτόν». Και αυτή η ερώτηση δεν ήταν κραυγή αμφισβήτησης. Ήταν ψίθυρος δυνατότητας. Και ο ψίθυρος αυτός δεν ήρθε απ’ έξω. Τον άκουσα μέσα μου.
Η σιωπή πριν από την πτώση δεν με προστάτευε με τείχη. Με προστάτευε με πληρότητα. Όταν όμως η πληρότητα άρχισε να φαίνεται ως κάτι που μπορεί να συμπληρωθεί, τότε η σιωπή άρχισε να χάνει την εξουσία της. Όχι γιατί έγινε αδύναμη, αλλά γιατί εγώ έπαψα να της αρκούμαι. Και αυτή η στιγμή δεν ήταν ηθική πτώση. Ήταν υπαρξιακή μετατόπιση.
Δεν ένιωσα ενοχή. Δεν ένιωσα φόβο. ένιωσα δυνατότητα. Και η δυνατότητα αυτή ήταν η αρχή της διάσπασης. Γιατί μέχρι τότε δεν υπήρχαν επιλογές. Υπήρχε σχέση. Όταν όμως άρχισα να σκέφτομαι ότι μπορώ να ακούσω και αλλιώς, τότε η σιωπή έπαψε να είναι αυτονόητη. Έγινε ένα ενδεχόμενο ανάμεσα σε άλλα.
Εκείνη τη στιγμή γεννήθηκε μέσα μου ο χώρος για λόγο. Όχι για τον λόγο του Θεού, αλλά για λόγο περί του Θεού. Και αυτός ο χώρος δεν ήταν ακόμη αμαρτία. Ήταν προετοιμασία. Ήταν το άνοιγμα της συνείδησης ως σκηνής. Ήταν η πρώτη φορά που ο άνθρωπος έγινε ακροατής αντί για μέτοχος. Και όταν ο άνθρωπος γίνεται ακροατής, τότε κάποιος άλλος μπορεί να μιλήσει.
Η σιωπή πριν από την πτώση δεν χάθηκε μονομιάς. Υποχώρησε. Και μέσα σε αυτή την υποχώρηση, γεννήθηκε η πρώτη απόσταση. Όχι από τον Θεό, αλλά από την πληρότητα. Και εκεί, σε αυτή την απόσταση, άρχισε να σχηματίζεται η ανάγκη για ερμηνεία. Όταν αρχίζεις να ερμηνεύεις τη ζωή, έχεις ήδη βγει από αυτήν.
Αυτή ήταν η στιγμή πριν από την πτώση. Όχι η παράβαση. Όχι ο καρπός. Αλλά η στιγμή που η σιωπή έπαψε να είναι αρκετή. Και όταν η σιωπή παύει να αρκεί, τότε κάποιος άλλος θα προσφερθεί να μιλήσει.
Προοίμιο ΙΙΙ – Η Σιωπή πριν από την Πτώση
Η σιωπή πριν από την πτώση δεν ήταν αδύναμη. Δεν ηττήθηκε. Παραδόθηκε από μέσα. Όχι γιατί δεν άντεξε, αλλά γιατί εγώ άρχισα να την αντιμετωπίζω σαν κάτι που μπορεί να αντικατασταθεί. Και αυτή είναι η πιο λεπτή και πιο επικίνδυνη μορφή απώλειας: όχι η βίαιη ρήξη, αλλά η εσωτερική υποκατάσταση.
Δεν θυμάμαι τη στιγμή που είπα «όχι» στον Θεό. Θυμάμαι τη στιγμή που άρχισα να σκέφτομαι ότι ίσως υπάρχει και κάτι άλλο να ακουστεί. Κάτι που δεν θα αναιρούσε τη σιωπή, αλλά θα τη συμπλήρωνε. Και αυτή η σκέψη δεν φαινόταν εχθρική. Φαινόταν λογική. Φαινόταν ώριμη. Φαινόταν σαν βήμα προς τη γνώση. Εκεί ακριβώς κρύβεται η πλάνη.
Η σιωπή δεν χάνεται όταν την αρνείσαι. Χάνεται όταν την ερμηνεύεις. Όταν την κάνεις αντικείμενο σκέψης αντί για χώρο ζωής. Όταν αρχίζεις να τη μετράς, να τη συγκρίνεις, να τη ζυγίζεις. Τότε παύει να είναι σιωπή και γίνεται φόντο. Και πάνω σε αυτό το φόντο μπορεί να σταθεί κάθε ξένος λόγος.
Εκεί γεννήθηκε μέσα μου η πρώτη διάσπαση. Όχι ως αμαρτία, αλλά ως αυτοσυνείδηση. Για πρώτη φορά στάθηκα απέναντι στον εαυτό μου. Και αυτή η στάση δεν ήταν ακόμη εγωισμός. Ήταν απορία. Αλλά η απορία, όταν δεν γεννιέται από τον Θεό, γίνεται ρωγμή. Και η ρωγμή γίνεται είσοδος.
Αρχισα να αισθάνομαι ότι υπάρχω ως κάτι ξεχωριστό. Όχι ακόμη αποκομμένο, αλλά διακριτό. Και αυτή η διάκριση με έκανε να θέλω να ακούσω. Να μου μιλήσει κάποιος. Να μου εξηγήσει. Να μου αποκαλύψει. Η σιωπή δεν εξηγεί. Απλώς είναι. Και εγώ, για πρώτη φορά, δεν αρκέστηκα στο «είναι».
Έτσι προετοιμάστηκε ο χώρος. Όχι ο εξωτερικός, αλλά ο εσωτερικός. Η συνείδηση άρχισε να μοιάζει με σκηνή που περιμένει λόγο. Και όταν μια σκηνή είναι έτοιμη, ο ηθοποιός θα εμφανιστεί. Όχι με κραυγή, αλλά με ρόλο. Όχι ως εχθρός, αλλά ως λειτουργός. Όχι ως βία, αλλά ως πρόσκληση.
Η σιωπή πριν από την πτώση δεν καταργήθηκε. Σπρώχτηκε στο βάθος. Και αυτό το βάθος έγινε η πρώτη λήθη. Όχι λήθη του Θεού, αλλά λήθη της κοινωνίας. Από εκεί και πέρα, ο άνθρωπος δεν ζει. Ακούει για να ζήσει. Δεν κοινωνεί. Επιλέγει. Δεν είναι. Αποφασίζει.
Αυτή είναι η τελευταία στιγμή πριν από την πτώση. Η στιγμή που η σιωπή υπάρχει ακόμη, αλλά δεν κυβερνά. Η στιγμή που ο άνθρωπος στέκεται έτοιμος να δεχτεί λόγο. Όχι τον λόγο που γεννά ζωή, αλλά τον λόγο που υπόσχεται περισσότερη ζωή. Και όταν η υπόσχεση μπει στη θέση της παρουσίας, τότε η τελεσιουργία μπορεί να αρχίσει.
Εκεί τελειώνει η σιωπή. Όχι γιατί χάθηκε ο Θεός, αλλά γιατί εγώ έπαψα να κατοικώ μέσα Του. Και τότε, χωρίς θόρυβο, χωρίς φωτιά, χωρίς σεισμό, ανοίγει το στόμα εκείνου που περίμενε. Και μιλά.
Μέρος Ι – Ο Όφις ως Ιερέας
Η ιερατική στάση του όφεως – Δεν επιτίθεται· τελεί
Ο όφις δεν εμφανίζεται ως θηρίο. Δεν εισβάλλει. Στέκεται. Και η στάση του είναι το πρώτο σημείο ότι δεν έχουμε να κάνουμε με επίθεση, αλλά με τελετή. Δεν έρχεται ως εχθρός, αλλά ως λειτουργός. Δεν υψώνει φωνή, αλλά λόγο. Και ο λόγος του δεν είναι κραυγή, αλλά πρόσκληση. Εκεί αρχίζω να καταλαβαίνω: η πτώση δεν ξεκινά με βία, αλλά με ιερατική ακρίβεια.
Ο όφις στέκεται όπως στέκεται ο ιερέας: ανάμεσα. Όχι απέναντι στον Θεό, αλλά ανάμεσα στον Θεό και στον άνθρωπο. Δεν ακυρώνει ευθέως τον Θεό. Τον ερμηνεύει. Και αυτό είναι το πιο επικίνδυνο σημείο. Ο ψευδο-ιερέας δεν λέει «ο Θεός δεν υπάρχει». Λέει «ο Θεός εννοούσε κάτι άλλο». Έτσι δεν γκρεμίζει τον ναό· τον μετατρέπει.
Δεν με πιέζει. Δεν με φοβίζει. Δεν με απειλεί. Με κοιτά και μου μιλά σαν να με σέβεται. Σαν να αναγνωρίζει τη νοημοσύνη μου. Σαν να μου δίνει θέση συνομιλητή. Και εκεί νιώθω για πρώτη φορά κάτι να αλλάζει: δεν είμαι πλέον μέτοχος της ζωής, αλλά ερμηνευτής της. Ο όφις με ανεβάζει στο αναλόγιο. Μου δίνει ρόλο. Και ο ρόλος είναι πάντα παγίδα.
Η ιερατική του στάση φαίνεται στον τρόπο που χειρίζεται τον λόγο. Δεν δηλώνει. Ρωτά. Δεν αποκαλύπτει. Υποβάλλει. Δεν προσφέρει καρπό· προετοιμάζει την όρεξη. Όπως κάθε τελετουργία, δεν αρχίζει από την πράξη, αλλά από τη διάθεση. Όχι από το χέρι, αλλά από τη συνείδηση. Και η συνείδησή μου αρχίζει να κινείται όπως κινείται ο πιστός μπροστά στο μυστήριο: με δέος, με προσδοκία, με επιθυμία συμμετοχής.
Ο όφις δεν βιάζεται. Η τελεσιουργία χρειάζεται χρόνο. Χρειάζεται συγκατάθεση. Χρειάζεται να σταθώ μόνος μου απέναντι στον λόγο του και να πω μέσα μου «ναι». Και αυτό το «ναι» δεν είναι κραυγή αμαρτίας. Είναι λεπτή μετατόπιση εμπιστοσύνης. Αρχίζω να τον ακούω όχι σαν εχθρό, αλλά σαν γνώστη. Σαν κάποιον που ξέρει κάτι παραπάνω. Και εκεί ο ιερέας έχει ήδη κερδίσει.
Καταλαβαίνω τότε ότι η πτώση δεν είναι παράβαση εντολής. Είναι αλλαγή λειτουργού. Αλλάζω ποιος μου μιλά για τον Θεό. Αλλάζω ποιος ερμηνεύει τη ζωή. Ο όφις δεν μου λέει να φύγω από τον Θεό. Μου λέει να Τον ξανασκεφτώ. Και αυτό είναι αρκετό για να αλλάξει όλο το πλαίσιο της ύπαρξης.
Δεν επιτίθεται. Τελεί. Τελεί μια αντεστραμμένη λειτουργία όπου ο Θεός γίνεται αντικείμενο λόγου και ο άνθρωπος γίνεται κέντρο κρίσης. Και εγώ, χωρίς να το καταλάβω, παύω να είμαι κοινωνός και γίνομαι κριτής. Ο όφις έχει τελειώσει το έργο του πριν ακόμη αγγίξω τον καρπό. Γιατί η πραγματική τελεσιουργία έχει ήδη συντελεστεί μέσα μου.
Μέρος ΙΙ – Η Υποβολή ως Λειτουργική Πράξη
Η υποβολή όχι ως ψυχολογικό τέχνασμα, αλλά ως πράξη λατρείας – Πώς λειτουργεί
Η υποβολή δεν είναι κόλπο. Δεν είναι τεχνική χειρισμού. Δεν είναι παιχνίδι μυαλού. Αυτά είναι φτωχές ερμηνείες για κάτι πολύ βαθύτερο. Η υποβολή είναι λειτουργία. Και όπως κάθε λειτουργία, έχει ρυθμό, τάξη, στάδια και σκοπό. Όταν το κατάλαβα αυτό, έπαψα να βλέπω την πτώση ως αδυναμία χαρακτήρα και άρχισα να τη βλέπω ως πλήρη τελεσιουργία.
Η υποβολή λειτουργεί πρώτα αφαιρώντας. Δεν προσθέτει αμέσως κάτι νέο. Αφαιρεί τη βεβαιότητα. Όχι με άρνηση, αλλά με ερώτηση. Η ερώτηση δεν είναι ουδέτερη. Είναι ιερατικό εργαλείο. Όπως ο ιερέας καλεί τον πιστό να στραφεί προς το άγιο, έτσι η υποβολή καλεί τη συνείδηση να στραφεί προς το ενδεχόμενο. Και το ενδεχόμενο είναι πάντα ρήγμα στην πληρότητα.
Δεν μου λέει «αυτό είναι ψέμα». Μου λέει «είσαι σίγουρος;». Και μόλις η βεβαιότητα μετατραπεί σε θέμα προς εξέταση, η λατρεία έχει ήδη αλλάξει αντικείμενο. Δεν λατρεύω πια την παρουσία. Λατρεύω τη δυνατότητα. Δεν ζω πια. Σκέφτομαι για να ζήσω. Και αυτό είναι η πρώτη λειτουργική μετατόπιση.
Η υποβολή έχει και χώρο. Δεν γίνεται στο σώμα. Γίνεται στη συνείδηση. Η συνείδηση μετατρέπεται σε αγία τράπεζα, όχι γιατί είναι ιερή, αλλά γιατί γίνεται τόπος τελετής. Εκεί ακουμπά ο λόγος. Εκεί αναπαύεται η σκέψη. Εκεί ωριμάζει η επιθυμία. Η υποβολή δεν με ωθεί να πράξω. Με οδηγεί να αποδεχτώ. Και η αποδοχή είναι πάντα πιο βαθιά από την πράξη.
Όπως κάθε λατρεία, έτσι και αυτή έχει αντικείμενο. Το αντικείμενο δεν είναι ο καρπός. Είναι η αυτονομία. Η υποβολή μου ψιθυρίζει ότι μπορώ να σταθώ μόνος μου απέναντι στην αλήθεια. Ότι μπορώ να την αξιολογήσω. Να την γευτώ χωρίς κοινωνία. Να την κατέχω. Και εκεί η λατρεία ολοκληρώνεται: όταν ο άνθρωπος γίνει μέτρο.
Η υποβολή λειτουργεί χωρίς βιασύνη. Δεν απαιτεί άμεση ανταπόκριση. Περιμένει. Ο χρόνος είναι μέρος της τελετής. Όπως σε κάθε λειτουργία, υπάρχει προετοιμασία, αναμονή, σιωπή. Και μέσα σε αυτή τη σιωπή, η επιθυμία δεν φαίνεται ακόμη αμαρτωλή. Φαίνεται φυσική. Φαίνεται ώριμη. Φαίνεται δικαιολογημένη.
Κατάλαβα τότε ότι η υποβολή δεν είναι εχθρός της ελευθερίας. Είναι η παραχάραξή της. Δεν μου αφαιρεί την επιλογή. Μου αλλάζει το πλαίσιο μέσα στο οποίο επιλέγω. Και όταν το πλαίσιο αλλάξει, η επιλογή είναι ήδη καθορισμένη. Η λατρεία έχει ήδη συντελεστεί.
Η πτώση δεν αρχίζει όταν απλώνω το χέρι. Αρχίζει όταν σκύβω με τον νου. Όταν δέχομαι να λειτουργήσει μέσα μου ένας άλλος λόγος. Όχι ως βία, αλλά ως λατρεία. Και τότε καταλαβαίνω: η υποβολή είναι η πιο επιτυχημένη λειτουργική πράξη, γιατί δεν φαίνεται ποτέ ως τέτοια. Και όμως, εκεί, μέσα στη σιωπηλή της ακρίβεια, γεννιέται ο πρώτος ψευδο-ναός. Μέσα μου.
Μέρος ΙΙΙ – Η Συνείδηση ως Αγία Τράπεζα
Ο χώρος όπου τελείται η τελεσιουργία – Όχι έξω από εμένα· μέσα σε εμένα
Η τελεσιουργία δεν χρειάζεται τόπο εξωτερικό. Δεν στήνεται σε ναό από πέτρα. Δεν απαιτεί βωμό ορατό. Ο τόπος της είναι η συνείδηση. Εκεί τελείται ό,τι δεν φαίνεται. Εκεί συντελείται η πιο κρίσιμη μετατόπιση της ύπαρξης. Όχι έξω από εμένα· μέσα σε εμένα. Και αυτό είναι που κάνει την πτώση τόσο βαθιά και τόσο καθολική.
Η συνείδηση δεν είναι ουδέτερο πεδίο. Δεν είναι απλώς μηχανισμός σκέψης. Είναι χώρος σχέσης. Όταν κατοικείται από τον Θεό, είναι τόπος κοινωνίας. Όταν όμως αποσπαστεί από την κοινωνία και στραφεί προς τον εαυτό της, γίνεται τόπος τελετής. Και κάθε τόπος τελετής ζητά λειτουργό. Ο όφις το γνωρίζει αυτό. Γι’ αυτό δεν χτίζει έξω. Εισέρχεται μέσα.
Στη συνείδηση ακουμπά ο λόγος του. Όχι σαν εντολή, αλλά σαν σπόρος. Και η συνείδηση, από χώρος ακρόασης του Θεού, μετατρέπεται σε χώρο επεξεργασίας λόγων. Αρχίζω να ζυγίζω. Να συγκρίνω. Να εξετάζω. Και αυτή η εξέταση μοιάζει με ωριμότητα, αλλά είναι ήδη αλλοίωση. Γιατί εκεί που υπήρχε εμπιστοσύνη, τώρα υπάρχει κρίση.
Η αγία τράπεζα δεν είναι άγια από μόνη της. Αγιάζεται από Αυτόν που κοινωνείται. Όταν όμως αλλάξει το περιεχόμενο, αλλάζει και ο χαρακτήρας της. Η συνείδησή μου γίνεται αγία τράπεζα ψευδούς λειτουργίας, γιατί πάνω της δεν προσφέρεται πια η ζωή, αλλά η ιδέα της ζωής. Δεν κοινωνώ. Καταναλώνω σκέψη.
Εκεί τελείται η πιο ύπουλη πράξη: η αντικατάσταση της παρουσίας με ερμηνεία. Δεν ζω τον Θεό. Τον σκέφτομαι. Δεν Τον αναπνέω. Τον αξιολογώ. Και κάθε αξιολόγηση απαιτεί απόσταση. Η απόσταση αυτή είναι το πρώτο ρήγμα. Και μέσα σε αυτό το ρήγμα, η τελεσιουργία προχωρά χωρίς αντίσταση.
Η συνείδηση αρχίζει να λειτουργεί όπως ο πιστός μπροστά στο μυστήριο, αλλά χωρίς Θεό. Σκύβει. Περιμένει. Επιθυμεί. Όχι πια την κοινωνία, αλλά τη γνώση. Και η γνώση αυτή δεν είναι φως. Είναι βάρος. Γιατί με κάνει υπεύθυνο χωρίς να με κάνει ζωντανό. Με κάνει κριτή χωρίς να με κάνει σοφό.
Καταλαβαίνω τότε ότι η πτώση δεν είναι πράξη ανυπακοής, αλλά πράξη λατρείας σε λάθος τόπο. Λατρεύω μέσα μου κάτι άλλο. Τη δυνατότητα να είμαι το μέτρο. Τη δυνατότητα να αποφασίζω μόνος μου τι είναι καλό και τι κακό. Και η συνείδηση, αντί να είναι τόπος συνάντησης, γίνεται θρόνος.
Ο όφις δεν χρειάζεται να με σπρώξει. Μου έχει ήδη δώσει χώρο. Και εγώ, χωρίς να το καταλάβω, έχω ήδη μετατρέψει την καρδιά μου σε ναό άλλης λειτουργίας. Όλα έχουν τελειώσει πριν ακόμη αγγίξω τον καρπό. Γιατί η τελεσιουργία δεν γίνεται με τα χέρια, αλλά με τη συγκατάθεση της συνείδησης. Και αυτή η συγκατάθεση δόθηκε εντός μου.
Μέρος IV – Τα Σκεύη του Ψεύδους
Λόγος, ερώτηση, αμφιβολία ως ιερατικά σκεύη – Κατάθεση ψυχής
Δεν ήρθαν τα σκεύη του ψεύδους σαν όπλα. Ήρθαν σαν εργαλεία καθαρά, σχεδόν σεβαστικά. Δεν γυάλιζαν από κακία, αλλά από λογικότητα. Και γι’ αυτό τα δέχτηκα. Ο λόγος, η ερώτηση, η αμφιβολία δεν μου παρουσιάστηκαν ως εχθροί της πίστης, αλλά ως συνοδοί της. Και εκεί ακριβώς άρχισαν να λειτουργούν.
Ο λόγος ήταν το πρώτο σκεύος. Όχι ο λόγος που γεννά ζωή, αλλά ο λόγος που εξηγεί τη ζωή. Αρχισα να μιλάω για τον Θεό αντί να ζω ενώπιόν Του. Ο λόγος μου έγινε μετρημένος, προσεκτικός, ορθολογικός. Και όσο πιο σωστά μιλούσα, τόσο λιγότερο προσευχόμουν. Δεν το κατάλαβα αμέσως. Ο λόγος μου έδινε την αίσθηση ότι πλησιάζω την αλήθεια, ενώ στην πραγματικότητα την αντικαθιστούσα.
Μετά ήρθε η ερώτηση. Όχι η κραυγή του πόνου, αλλά η ερώτηση της ανάλυσης. «Γιατί έτσι;» «Μήπως αλλιώς;» «Είσαι βέβαιος;». Η ερώτηση δεν ζητούσε απάντηση από τον Θεό. Τη ζητούσε από εμένα. Και έτσι άρχισα να στέκομαι ως κριτής του Θεού. Όχι εχθρικά, αλλά ώριμα, όπως νόμιζα. Η ερώτηση έγινε το σκεύος που άνοιξε τον χώρο για να μπει η αμφιβολία.
Η αμφιβολία δεν ήρθε σαν άρνηση. Ήρθε σαν προσοχή. Σαν σύνεση. Σαν ταπεινότητα. Μου ψιθύριζε ότι ίσως δεν τα ξέρω όλα. Και αυτό ήταν αλήθεια. Αλλά η αμφιβολία δεν με οδήγησε στην εμπιστοσύνη. Με οδήγησε στην αυτοαναφορά. Άρχισα να στηρίζομαι στον νου μου για να σταθώ. Και ο νους, όσο κι αν φαίνεται δυνατός, δεν αντέχει το βάρος της αλήθειας.
Αυτά τα τρία σκεύη λειτούργησαν μέσα μου σαν ιερατική ακολουθία. Πρώτα ο λόγος, μετά η ερώτηση, έπειτα η αμφιβολία. Και στο τέλος, η απόφαση. Όχι να αρνηθώ τον Θεό, αλλά να Τον κρατήσω υπό έλεγχο. Να Τον χωρέσω σε έννοιες. Να Τον κάνω διαχειρίσιμο. Εκεί κατάλαβα ότι η τελεσιουργία είχε προχωρήσει βαθιά.
Καταθέτω την ψυχή μου εδώ χωρίς δικαιολογία. Δεν με έριξαν. Συμμετείχα. Δεν με εξαπάτησαν με ψέμα κραυγαλέο. Με μύησαν με λεπτότητα. Τα σκεύη του ψεύδους δεν είναι βρώμικα. Είναι καθαρά, καλογυαλισμένα, έτοιμα για χρήση. Και γι’ αυτό είναι επικίνδυνα.
Σήμερα τα αναγνωρίζω μέσα μου. Όταν ο λόγος μου προηγείται της σιωπής. Όταν η ερώτηση προηγείται της εμπιστοσύνης. Όταν η αμφιβολία προηγείται της προσευχής. Τότε ξέρω: τα σκεύη έχουν τοποθετηθεί ξανά στην αγία τράπεζα της συνείδησής μου. Και η τελεσιουργία καραδοκεί. Όχι έξω από εμένα· μέσα σε εμένα.
Μέρος V – Ο Καρπός ως Αντίδωρο Θανάτου
Η κατανάλωση δεν είναι πράξη γνώσης, αλλά κοινωνία – Αλληγορία μαχόμενης ψυχής
Ο καρπός δεν είναι πληροφορία. Δεν είναι δεδομένο. Δεν είναι γνώση προς απόκτηση. Ο καρπός είναι προσφορά. Και κάθε προσφορά, όταν λαμβάνεται, γίνεται κοινωνία. Αυτό κατάλαβα αργά, όταν πια το στόμα είχε κλείσει και η πίκρα είχε απλωθεί σε όλο το σώμα. Δεν έφαγα για να μάθω. Εφαγα για να ενωθώ. Και ενώ νόμιζα πως κοινωνώ γνώση, κοινώνησα θάνατο.
Η αλληγορία είναι σκληρή, αλλά αληθινή. Ο καρπός δόθηκε σαν αντίδωρο. Όχι ως δώρο ζωής, αλλά ως μίμηση δώρου. Όπως το αντίδωρο μοιάζει με άρτο αλλά δεν είναι Σώμα, έτσι και ο καρπός έμοιαζε με σοφία αλλά δεν ήταν ζωή. Ήταν το ίχνος μιας λειτουργίας χωρίς Θεό. Και εγώ τον δέχτηκα, όχι ως πεινασμένος, αλλά ως μυημένος.
Η κατανάλωση δεν έγινε με βιασύνη. Δεν άρπαξα. Προσέλαβα. Με ευλάβεια σχεδόν. Με τη σοβαρότητα εκείνου που πιστεύει πως κάνει κάτι σημαντικό. Και αυτή η σοβαρότητα είναι το πιο επικίνδυνο σημείο. Γιατί η αμαρτία που γίνεται με ελαφρότητα πληγώνει λιγότερο από εκείνη που γίνεται με τελετουργική βεβαιότητα.
Μέσα μου ένιωσα να αλλάζει κάτι αμέσως. Όχι φως. Όχι δύναμη. Αλλά βάρος. Ένα βάρος αυτογνωσίας που δεν οδηγεί στη μετάνοια, αλλά στην αυτοδικαίωση. Έγινα γνώστης χωρίς να γίνω ζωντανός. Έγινα κριτής χωρίς να γίνω καθαρός. Ο καρπός δεν με άνοιξε προς τον Θεό. Με έκλεισε μέσα μου.
Η μαχόμενη ψυχή μου φωνάζει τώρα αυτό που τότε δεν ήξερα να πει: δεν υπάρχει ουδέτερη κατανάλωση. Ό,τι τρώω με τρώει. Ό,τι κοινωνώ με κοινωνεί. Και όταν κοινωνώ κάτι που δεν είναι ζωή, τότε ο θάνατος δεν έρχεται ως τιμωρία, αλλά ως φυσική συνέπεια. Ο καρπός δεν σκότωσε. Αποσύνδεσε.
Ήταν αντίδωρο θανάτου, γιατί δεν είχε πηγή. Δεν είχε πρόσωπο. Δεν είχε σχέση. Ήταν γνώση χωρίς αγάπη. Και η γνώση χωρίς αγάπη δεν φωτίζει. Διαχωρίζει. Με χώρισε από τον Θεό, όχι επειδή Εκείνος έφυγε, αλλά επειδή εγώ έπαψα να Τον αναζητώ ως Ζωή. Τον αναζήτησα ως έννοια.
Σήμερα, με μαχόμενη ψυχή, στέκομαι απέναντι σε κάθε καρπό που μου προσφέρεται χωρίς πρόσωπο. Σε κάθε γνώση που δεν ζητά σχέση. Σε κάθε αλήθεια που δεν γεννά ζωή. Και ομολογώ: η πτώση δεν ήταν μια μπουκιά. Ηταν μια κοινωνία. Και ο αγώνας δεν είναι να μην ξαναφάω, αλλά να κοινωνώ μόνο Εκείνον που είναι η Ζωή. Γιατί μόνο Εκείνος δεν δίνει αντίδωρο θανάτου, αλλά Σώμα που ανασταίνει.
Μέρος VI – Η Γέννηση του Ατόμου
Από κοινωνός σε άτομο – Η ολοκλήρωση της δαιμονικής τελεσιουργίας
Η τελεσιουργία ολοκληρώνεται όταν γεννιέται το άτομο. Όχι ο άνθρωπος. Το άτομο. Εκείνος που αποκόπηκε από τη σχέση και στάθηκε μόνος απέναντι στον εαυτό του. Δεν έγινε αυτό με κραυγή. Έγινε με συνέπεια. Με μια αλυσίδα πράξεων που έμοιαζαν λογικές, ώριμες, αναγκαίες. Και όταν τελείωσε, δεν υπήρχε πια κοινωνός. Υπήρχε υποκείμενο.
Μέχρι εκείνη τη στιγμή ζούσα από τη σχέση. Η ταυτότητά μου δεν ήταν κάτι που έπρεπε να ορίσω. Ήταν δοσμένη μέσα στην κοινωνία. Όταν όμως κοινώνησα τον καρπό, άρχισα να υπάρχω ως κέντρο. Όχι ως πρόσωπο, αλλά ως σημείο αναφοράς. Η ζωή έπαψε να έρχεται σε μένα. Έπρεπε να την αποκτήσω. Και ό,τι αποκτάται, μετριέται. Και ό,τι μετριέται, χάνεται.
Η γέννηση του ατόμου δεν είναι ενδυνάμωση. Είναι συρρίκνωση. Μοιάζει με αυτονομία, αλλά είναι απομόνωση. Μοιάζει με ελευθερία, αλλά είναι βάρος. Γιατί το άτομο πρέπει να κουβαλήσει μόνο του αυτό που πριν του δινόταν ως χάρη. Πρέπει να αποφασίζει, να κρίνει, να ορίζει. Και όσο περισσότερο ορίζει, τόσο λιγότερο ζει.
Έγινα άτομο τη στιγμή που άρχισα να λέω «εγώ». Όχι ως μαρτυρία ύπαρξης, αλλά ως όριο. Εγώ και ο Θεός. Εγώ και ο άλλος. Εγώ και η αλήθεια. Η κοινωνία διασπάστηκε σε σχέσεις διαπραγμάτευσης. Και εκεί όπου υπήρχε αγάπη, μπήκε σύγκριση. Εκεί όπου υπήρχε δωρεά, μπήκε δικαίωμα.
Αυτή είναι η τελική πράξη της δαιμονικής τελεσιουργίας: να με πείσει ότι υπάρχω πληρέστερα μόνος. Όχι εναντίον του Θεού, αλλά χωρίς Τον Θεό ως Ζωή. Με τον Θεό ως ιδέα. Ως έννοια. Ως θέμα σκέψης. Και έτσι μπορώ να Τον σκέφτομαι χωρίς να Τον χρειάζομαι. Να μιλώ για Εκείνον χωρίς να ζω από Εκείνον.
Το άτομο γεννιέται όταν η συνείδηση γίνεται κλειστό σύστημα. Όταν δεν περιμένει πια ζωή απ’ έξω, αλλά παράγει νόημα από μέσα. Και αυτό το νόημα, όσο λαμπρό κι αν φαίνεται, είναι θνησιγενές. Γιατί δεν τρέφεται από κοινωνία. Τρέφεται από τον εαυτό του. Και ο εαυτός, όταν γίνεται τροφή, τελειώνει.
Στέκομαι σήμερα απέναντι σε αυτή τη γέννηση και την ονομάζω. Δεν τη δικαιολογώ. Δεν τη ρομαντικοποιώ. Ήταν η ολοκλήρωση της πτώσης. Όχι η αρχή της ελευθερίας. Ήταν η στιγμή που έπαψα να είμαι άνθρωπος εν σχέσει και έγινα άτομο εν απομονώσει. Και από τότε ο κόσμος γέμισε άτομα που πεινούν για κοινωνία και χτίζουν ναούς για να καλύψουν την απουσία της.
Η τελεσιουργία ολοκληρώθηκε. Αλλά δεν είναι το τέλος. Γιατί ό,τι γεννήθηκε ως άτομο μπορεί να ξαναγεννηθεί ως πρόσωπο. Όχι με γνώση, αλλά με επιστροφή. Όχι με ατομική απόφαση, αλλά με κοινωνία. Εκεί αρχίζει ο άλλος δρόμος. Όχι του όφεως, αλλά του Χριστού. Και εκεί, το άτομο πεθαίνει για να ζήσει ο άνθρωπος.
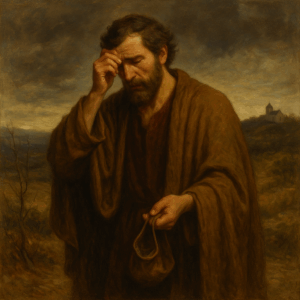
Επίλογος Ι – Η Μνήμη που Πονά
Η ανάμνηση της Εδέμ ως πληγή και ως κλήση
Η μνήμη της Εδέμ δεν με παρηγορεί. Με πονά. Δεν έρχεται σαν ανάμνηση φωτεινή, αλλά σαν ίχνος που καίει. Όχι γιατί θέλω να επιστρέψω ρομαντικά σε κάτι χαμένο, αλλά γιατί ξέρω ότι κάτι μέσα μου θυμάται ακόμα πώς ήταν να ζει χωρίς ρήγμα. Αυτή η μνήμη δεν είναι νοσταλγία. Είναι πληγή ανοιχτή που δεν κλείνει με εξηγήσεις.
Πονά γιατί δεν είναι παρελθόν. Αν ήταν παρελθόν, θα είχε τελειώσει. Πονά γιατί είναι παρούσα ως απουσία. Ως αίσθηση ότι κάτι λείπει και δεν αντικαθίσταται. Όσο κι αν γεμίσω τον κόσμο με λόγια, έργα, ναούς, ιδέες, η μνήμη της Εδέμ επιμένει. Σαν ψίθυρος που λέει: δεν ήταν έτσι η ζωή. Δεν ήταν διαχωρισμένη. Δεν ήταν βαριά.
Η μνήμη αυτή δεν με κατηγορεί. Με καλεί. Δεν μου δείχνει τον καρπό. Μου δείχνει τη σιωπή που προηγήθηκε. Και αυτή η σιωπή είναι το κριτήριο όλων. Όταν μιλώ πολύ, πονά. Όταν εξηγώ τα πάντα, πονά. Όταν στέκομαι μόνος μου και λέω «εγώ», πονά. Γιατί θυμάται ότι ήμουν κοινωνός πριν γίνω άτομο.
Υπάρχουν στιγμές που αυτή η μνήμη μοιάζει άδικη. Γιατί τι να την κάνω; Δεν μπορώ να γυρίσω πίσω. Δεν μπορώ να αναιρέσω την τελεσιουργία. Όμως τότε καταλαβαίνω κάτι βαθύτερο: η μνήμη δεν μου δόθηκε για να επιστρέψω μόνος. Μου δόθηκε για να αναγνωρίσω τον δρόμο. Όχι τον δρόμο της επιστροφής ως πράξη, αλλά τον δρόμο της θεραπείας ως σχέση.
Η ανάμνηση της Εδέμ είναι πληγή γιατί αποκαλύπτει το ψεύδος όλων των υποκατάστατων. Κάθε φορά που υπόσχομαι στον εαυτό μου πληρότητα χωρίς κοινωνία, πονά. Κάθε φορά που λατρεύω ιδέες αντί για πρόσωπα, πονά. Και αυτός ο πόνος δεν είναι τιμωρία. Είναι κλήση. Μου λέει ότι δεν είμαι φτιαγμένος για να ζω μόνος, ούτε για να σώζομαι μόνος.
Αρχίζω τότε να καταλαβαίνω ότι η μνήμη αυτή είναι δώρο. Σκληρό, αλλά αληθινό. Με κρατά σε εγρήγορση. Δεν με αφήνει να βολευτώ στην πτώση. Δεν με αφήνει να ονομάσω κανονικό αυτό που είναι τραύμα. Με αναγκάζει να κοιτάξω κατάματα το γεγονός ότι η ζωή χωρίς Θεό ως Ζωή δεν είναι απλώς φτωχότερη. Είναι άλλη ζωή.
Η μνήμη που πονά γίνεται έτσι μνήμη που οδηγεί. Όχι πίσω, αλλά μπροστά. Όχι προς την Εδέμ ως τόπο, αλλά προς την αποκατάσταση ως πρόσωπο. Δεν μου υπόσχεται επιστροφή στην αθωότητα. Μου υπόσχεται δυνατότητα ανάστασης. Και όσο πονά, ξέρω ότι ακόμα ζω. Γιατί μόνο ο ζωντανός θυμάται. Και μόνο όποιος θυμάται μπορεί να απαντήσει στην κλήση.
Επίλογος ΙΙ – Ο Χριστός ως Αληθινή Λειτουργία
Όχι αντίλογος, αλλά αντιστροφή της τελεσιουργίας – Όχι ψευδολατρεία, αλλά ζωή
Ο Χριστός δεν ήρθε να απαντήσει στον όφι. Δεν μπήκε σε διάλογο μαζί του. Δεν στάθηκε απέναντι στη δαιμονική τελεσιουργία για να την αντικρούσει με επιχειρήματα. Αν το έκανε, θα αναγνώριζε το έδαφός της. Ο Χριστός ήρθε για να την ανατρέψει εκ των έσω. Όχι με λόγο αντίθετο, αλλά με ζωή άλλη. Όχι με ερμηνεία, αλλά με παρουσία.
Καταλαβαίνω πια ότι ο Χριστός δεν είναι απάντηση στην πτώση. Είναι η κατάλυσή της. Δεν προσφέρει καλύτερη γνώση. Προσφέρει κοινωνία. Δεν διδάσκει απλώς τι είναι αλήθεια. Ειναι η Αλήθεια που κοινωνείται. Και αυτό αλλάζει τα πάντα. Γιατί εκεί όπου ο όφις μίλησε ως ψευδο-ιερέας, ο Χριστός προσφέρεται ως Αρχιερέας χωρίς λόγια περιττά. Με σάρκα. Με αίμα. Με σταυρό.
Η αντιστροφή της τελεσιουργίας δεν γίνεται στο επίπεδο της σκέψης. Γίνεται στο επίπεδο της ζωής. Εκεί όπου ο όφις έκανε τη συνείδηση αγία τράπεζα ψεύδους, ο Χριστός κάνει το σώμα Του Αγία Τράπεζα ζωής. Εκεί όπου εγώ έφαγα για να γίνω γνώστης, Εκείνος προσφέρεται για να με κάνει ζωντανό. Δεν μου ζητά να καταλάβω. Μου ζητά να κοινωνήσω.
Ο Χριστός δεν με καλεί να επιστρέψω στην Εδέμ. Με καλεί να περάσω από τον θάνατο. Γιατί μόνο ό,τι πεθαίνει ανασταίνεται. Το άτομο δεν σώζεται. Το άτομο πεθαίνει. Και μέσα από αυτόν τον θάνατο γεννιέται το πρόσωπο. Όχι αυτόνομο, αλλά ενωμένο. Όχι αυτάρκες, αλλά δεκτικό. Όχι κριτής, αλλά υιός.
Εδώ καταλαβαίνω τη διαφορά ανάμεσα στη ψευδολατρεία και στη ζωή. Η ψευδολατρεία με έκανε να σκύβω μέσα μου. Η ζωή με σηκώνει προς τον άλλον. Η ψευδολατρεία μου έδινε ρόλο. Η ζωή μου δίνει σχέση. Η ψευδολατρεία με έκανε να αποφασίζω. Η ζωή με κάνει να εμπιστεύομαι. Και αυτή η εμπιστοσύνη δεν είναι αδυναμία. Είναι ανάπαυση.
Ο Χριστός δεν καταργεί τη συνείδηση. Τη θεραπεύει. Δεν την κάνει ξανά αγία τράπεζα λόγων, αλλά τόπο μετάνοιας. Εκεί όπου παύω να τελώ μόνος μου. Εκεί όπου παραδίδω τον έλεγχο. Εκεί όπου δεν εξηγώ πια τον Θεό, αλλά Τον αφήνω να με ζήσει. Αυτή είναι η αληθινή λειτουργία. Όχι αυτή που τελώ εγώ, αλλά αυτή που με τελεί.
Και τότε καταλαβαίνω: η ζωή δεν είναι να μη φάω ποτέ ξανά. Είναι να κοινωνώ σωστά. Να κοινωνώ Εκείνον που δεν υπόσχεται θέωση, αλλά τη χαρίζει. Όχι ως ιδέα, αλλά ως σώμα. Όχι ως γνώση, αλλά ως ανάσταση. Έτσι η τελεσιουργία αντιστρέφεται. Όχι με άρνηση, αλλά με σταυρό. Όχι με ψευδολατρεία, αλλά με ζωή που νικά τον θάνατο.
Επίλογος ΙΙΙ – Μαρτυρία Μαχόμενης Ψυχής
Πρώτο πρόσωπο, χωρίς άμυνες – Πού στέκομαι. Τι ομολογώ. Γιατί δεν σιωπώ
Στέκομαι εδώ χωρίς άμυνες. Όχι γιατί δεν φοβάμαι, αλλά γιατί δεν αντέχω πια να κρύβομαι πίσω από λέξεις που δεν σώζουν. Δεν γράφω για να πείσω. Δεν γράφω για να νικήσω κάποιον. Γράφω γιατί αν σιωπήσω, θα προδώσω τη μνήμη που με κρατά ζωντανό. Και αυτή η μνήμη δεν είναι ιδέα. Είναι πληγή και χάρη μαζί.
Ομολογώ ότι γνώρισα την πτώση όχι ως θεωρία, αλλά ως τρόπο ζωής. Την έζησα μέσα μου. Την υπερασπίστηκα. Την έντυσα με επιχειρήματα. Την είπα ωριμότητα, ελευθερία, αυτογνωσία. Και όσο πιο πολύ την εξηγούσα, τόσο πιο μόνος γινόμουν. Δεν έπεσα μια φορά. Επεφτα κάθε μέρα, κάθε φορά που προτιμούσα τον έλεγχο από την εμπιστοσύνη, τον λόγο από τη σιωπή, το «εγώ» από το «μαζί».
Στέκομαι εδώ και ομολογώ ότι ο όφις δεν μου ήταν ξένος. Μου μιλούσε με φωνή γνώριμη. Με φωνή που έμοιαζε δική μου. Και αυτό ήταν το πιο επικίνδυνο. Γιατί όταν το ψεύδος μιλά σαν εσωτερική φωνή, δεν το πολεμάς. Το ακολουθείς. Και εγώ το ακολούθησα, μέχρι που η ζωή έγινε βάρος και η πίστη έννοια.
Δεν σιωπώ γιατί γνώρισα και την άλλη όχθη. Όχι ως θρίαμβο, αλλά ως έλεος. Γνώρισα τον Χριστό όχι σαν απάντηση στα ερωτήματά μου, αλλά σαν παρουσία που δεν ζητά εξηγήσεις. Εκεί που είχα μάθει να τελώ, Εκείνος με λύτρωσε από τον ρόλο. Εκεί που είχα μάθει να κρίνω, Εκείνος με έκανε να κλαίω. Και μέσα στα δάκρυα αυτά, άρχισε να ξαναγεννιέται ο άνθρωπος.
Ομολογώ ότι ακόμα μάχομαι. Δεν έγινα άτρωτος. Δεν έγινα καθαρός με μιας. Η τελεσιουργία αφήνει ίχνη. Αλλά τώρα τα αναγνωρίζω. Όταν ο λόγος μου γίνεται σκληρός, σταματώ. Όταν η σκέψη μου γίνεται θρόνος, υποχωρώ. Όταν η σιωπή επιστρέφει, ξέρω ότι βρίσκομαι ξανά στον σωστό δρόμο. Όχι γιατί τα κατάφερα, αλλά γιατί παραδόθηκα.
Δεν σιωπώ γιατί ο κόσμος είναι γεμάτος ψευδο-ναούς που μοιάζουν σωστοί. Γιατί η πτώση συνεχίζει να τελείται με άλλες λέξεις, άλλες στολές, άλλες λειτουργίες. Και αν δεν μιλήσω, θα μοιάσω με εκείνον που έφαγε και κρύφτηκε. Εγώ δεν θέλω να κρυφτώ άλλο. Θέλω να σταθώ γυμνός μπροστά στην Αλήθεια που δεν ντρέπεται για μένα.
Στέκομαι λοιπόν εδώ, μαχόμενη ψυχή, και ομολογώ: δεν σώθηκα από γνώση. Σώζομαι από σχέση. Δεν ζω από ερμηνεία. Ζω από κοινωνία. Και δεν σιωπώ γιατί αυτή η ζωή δεν μου ανήκει. Μου δόθηκε. Και ό,τι δίνεται, μαρτυρείται. Μέχρι τέλους.







Πρόσφατα Σχόλια